
MCI represents what researchers and clinicians regard as a “window” in which it may be possible to intervene and delay development to dementia. Moreover, it has been suggested that approximately 50% will progress to dementia in 5 years. Although 20–30% of persons with MCI will revert to normal at subsequent follow-up, there is a 5–10% annual rate of progression to dementia in those with MCI, which is much higher than the 1–2% incidence per year among the general population. Mild cognitive impairment (MCI), referring to cognitive decline from a previous level of functioning both subjectively and by objective evidence, represents the preclinical, transitional stage between healthy cognitive aging and dementia, and affects 10–15% of the population over the age of 65. Considering no effective treatment for dementia, as well as brain pathology which begins years before onset of objective cognitive symptoms and may be irreversible by the time of diagnosis, many investigators have shifted their focus toward delaying dementia in persons who are in preclinical phases of the disease. Both tools identify concordantly modifiable factors for MCI, which provide important evidence for establishing intervention measures.ĭementia is a leading cause of disability in people older than 65 years worldwide, including China, which induces huge challenges for policy makers, healthcare professionals, and family members. MCI prevalence is higher using MoCA compared to MMSE. MoCA is a better measure of cognitive function due to lack of ceiling effect and with good detection of cognitive heterogeneity. Increasing age (MMSE: OR = 2.073 for ≥75 years MoCA: OR = 1.869 for≥75 years), female (OR = 1.280 for MMSE OR = 1.163 for MoCA), living in county town (OR = 1.386 and 1.862 for MMSE and MoCA, respectively) or village (OR = 2.579 and 2.721 for MMSE and MoCA, respectively), smoking (OR = 1.373 and 1.288 for MMSE and MoCA, respectively), hypertension (MMSE: OR = 1.278 MoCA: OR = 1.208) and depression (MMSE: OR = 1.465 MoCA: OR = 1.350) were independently associated with greater likelihood of MCI compared to corresponding reference group in both scales (all p < 0.05). Percentage of relative standard deviation, the measure of inter-individual variance, for MoCA (26.9%) was greater than for MMSE (19.0%) overall ( p < 0.0001). Ceiling effect for MCI was less frequent using MoCA versus MMSE according to the distribution of total score. MMSE had good correlation with MoCA (Spearman correlation coefficient = 0.8374, p < 0.0001) and moderate agreement for detecting MCI with Kappa value of 0.5973 ( p < 0.0001).
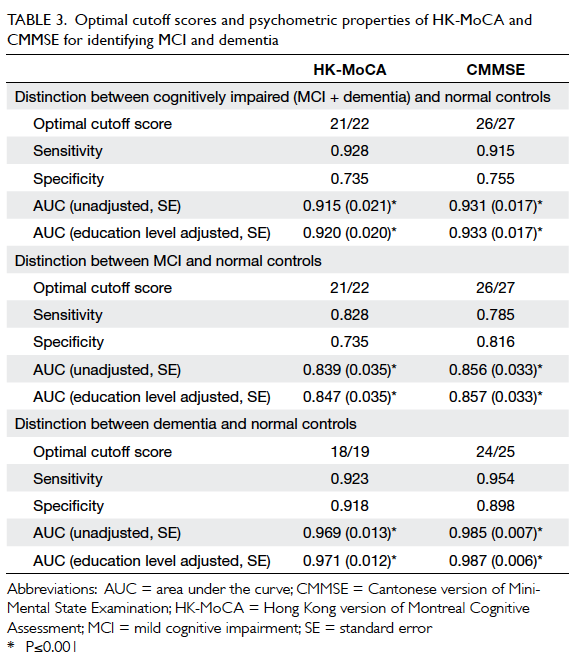
The overall MCI prevalence was 28.6% for MMSE and 36.2% for MoCA. Correlation and agreement for MCI between MMSE and MoCA were analyzed group differences in cognition were evaluated and multiple logistic regression model was used to clarify risk factors for MCI. Demographic and health-related characteristics were collected by questionnaires. Education-specific cutoffs of total score were used to diagnose MCI. Objective cognition was assessed by Chinese versions of MMSE and MoCA, and total score and subscores of cognitive domains were calculated for each. We conducted a cross-sectional analysis of 4923 adults aged ≥55 years from the Community-based Cohort Study on Nervous System Diseases. However, their comparison on which is best suited to assess cognition is scarce in samples from multiple regions of China.
Try to remember and tell me as many words as you can, including words you said the first time.” Put a check in the allocated space for each word the subject recalls after the second trial. When the subject indicates that (s)he has finished (has recalled all words), or can recall no more words, read the list a second time with the following instructions: “ I am going to read the same list for a second time. It doesn’t matter in what order you say them.” Mark a check in the allocated space for each word the subject produces on this first trial. When I am through, tell me as many words as you can remember. I am going to read a list of words that you will have to remember now and later on. Read a list of 5 words at a rate of 1 word per second, giving the following instructions: “ This is a memory test.


 0 kommentar(er)
0 kommentar(er)
